Causes of Genetic Hair Loss
Genetic Hair Loss in Men
Androgenetic alopecia (AGA) in men is the most common form of hair loss, affecting millions worldwide. By the age of 20, around 20% of men are already affected, and by the age of 50, every second man experiences some degree of hair loss. It typically begins with a receding hairline (receding temples) and can progress to complete baldness.
The main causes are:
- Dihydrotestosterone (DHT): The hormone dihydrotestosterone (DHT), a breakdown product of testosterone, plays a central role. It binds to androgen receptors in the hair follicles and causes progressive miniaturization of the follicles. As a result, the anagen phase (growth phase) shortens, and the hairs grow back thinner and weaker until they eventually fall out. DHT is produced through the activity of the enzyme 5-alpha-reductase, which exists in two types — Type I and Type II. It should be noted that inhibiting this enzyme naturally helps reduce hair loss.
- Genetic predisposition: Multiple genes, including the AR gene (androgen receptor gene), influence the sensitivity of hair follicles to dihydrotestosterone (DHT). Inheritance is polygenic, meaning both male and female relatives can be affected.
- Age: With increasing age, the effects of genetic factors and hormonal changes become more pronounced. In men, AGA often begins in their twenties or thirties.
Genetic Hair Loss in Women After Menopause
After menopause, women often experience diffuse hair thinning, especially along the midline of the scalp, without developing complete baldness. Up to 20% of women are affected even before menopause, and 40–50% after menopause.
This female pattern of hair loss has the following causes:
- Hormonal changes: The decline in estrogen production during menopause leads to a relative increase in androgen levels. As a result, the remaining estrogens can no longer balance the effects of androgens. In women with a genetic predisposition, this allows dihydrotestosterone (DHT) to exert a damaging effect on the hair follicles, resulting in a process similar to that seen in androgenetic alopecia.
- Genetic predisposition: As in men, genetic factors influence the susceptibility of hair follicles to the damaging effects of dihydrotestosterone (DHT). A familial pattern of diffuse hair loss is often observed in affected women.
- Age-related degeneration: In addition to hormonal changes, the regenerative capacity and cell division rate of hair follicles decrease with age.
- Stress and lifestyle: Additional factors such as stress, nutritional deficiencies, and reduced scalp blood circulation can further exacerbate hair loss.
Genetic Hair Loss in Women with PCOS
Polycystic ovary syndrome (PCOS) is a complex endocrine disorder that affects up to 10% of women of reproductive age and is often associated with androgenetic alopecia.
The main causes are:
- Hyperandrogenism: Women with PCOS often have elevated levels of androgens such as testosterone and dihydrotestosterone (DHT). When there is an increased sensitivity to DHT, it leads to miniaturization of the hair follicles — similar to androgenetic alopecia in men.
- Insulin resistance: Insulin resistance is another characteristic feature of PCOS. High insulin levels stimulate the ovaries to produce more androgens, which worsens hair loss.
- Inflammatory processes: Chronic low-grade inflammation, which often occurs in PCOS, can further damage the hair follicles.
- Genetic predisposition: PCOS also appears to have a genetic component that influences both insulin resistance and the sensitivity of hair follicles to androgens.
Similarities in the Causes of Hair Loss
Despite the different patterns of androgenetic alopecia in men and women, there are fundamental similarities in the underlying mechanisms:
- DHT as a central factor: In all three cases, dihydrotestosterone (DHT) plays a key role by damaging the hair follicles and accelerating their miniaturization.
- Genetic factors: A family history of hair loss is a major risk factor for all affected individuals. Genes influencing androgen sensitivity or susceptibility to hormonal imbalances are critical.
- Hormonal imbalances: In men, testosterone and dihydrotestosterone (DHT) are the main drivers, while in women, a relative increase in androgens (e.g., after menopause or due to PCOS) produces a similar effect.
- Hair follicle miniaturization: In all cases, hair follicles gradually shrink, leading to thinner and weaker hair growth until hair production eventually ceases.
Additionally, environmental factors such as stress, nutrition, and overall health can either exacerbate or mitigate these genetic and hormonal processes.

Prevention and Treatment of Hair Loss with Medication
The treatment of genetic hair loss includes several preventive and therapeutic approaches aimed at protecting hair follicles, improving blood circulation, and regulating hormonal factors. It is important to start treatment as early as possible: the longer genetically sensitive hair follicles are exposed to dihydrotestosterone (DHT), the longer the process of shrinkage and degeneration continues, and the more difficult it becomes to achieve regeneration.
Key medications and their mechanisms of action include:
Minoxidil
- Mechanism of action: The effect of Minoxidil was discovered by chance. This medication was originally developed to lower blood pressure. However, it was observed that men taking Minoxidil for hypertension experienced reduced hair loss and even regrowth in previously bald areas. Minoxidil acts as a vasodilator, improving blood circulation in the scalp. This increases the oxygen and nutrient supply to the hair follicles, prolonging the anagen (growth) phase and stimulating hair growth. However, Minoxidil has no hormonal effect and therefore does not counteract the sensitivity of hair follicles to dihydrotestosterone (DHT). As a result, its effectiveness is limited and it is not sufficient as a standalone treatment.
- Application: Minoxidil is available in topical form (solution or foam) and is applied directly to the affected areas of the scalp. It can also be injected into the scalp using fine needles.
- Long-term effect: Consistent and regular use is essential, as the effect naturally diminishes once the medication is discontinued.
Botox
- Mechanism of action: We all know Botox from aesthetic medicine — it is a bacterial toxin that competitively inhibits the neurotransmitter acetylcholine. Simply put, at the junction where nerve impulses are transmitted to the muscle, the Botox molecule displaces acetylcholine, thereby reducing or completely blocking signal transmission to the muscle. This is the basic principle behind wrinkle reduction with Botox. Wrinkles form due to the contraction of muscles located just beneath the skin (crow’s feet, frown lines, forehead lines, etc.). Through repeated muscle contractions in daily life and the natural loss of skin elasticity with age, skin folds form at 90° angles to the direction of muscle movement.
In the human scalp, there are several strong muscles beneath the skin, including the frontalis muscle (forehead elevator), the masseter muscle (jaw muscle), and the neck muscles. Due to stress, many people have chronically increased muscle tension in these areas, which causes the scalp to remain under constant tension and consequently reduces blood flow to the hair follicles. Relaxing these muscles improves scalp blood circulation and therefore the oxygen and nutrient supply to the hair follicles, creating a more favorable environment for hair growth.
As a side note: reducing muscle tension is also a therapeutic approach to migraine treatment when, as is often the case, the cause is compression of sensitive nerves in the skull area. Minoxidil and Botox therefore have synergistic mechanisms of action — both improve blood circulation to the scalp: Minoxidil by dilating blood vessels and Botox by reducing muscle tension and thus decreasing vascular compression in the scalp.
Application: Botox is injected into specific points of the scalp and is particularly promising for stress-related hair loss.
Finasteride
- Mechanism of action: Finasteride inhibits 5-alpha-reductase, an enzyme responsible for converting testosterone into dihydrotestosterone (DHT). This reduces DHT levels, thereby slowing down or stopping the miniaturization of hair follicles.
- Application: Administered orally in tablet form or via injection into the scalp using a very fine needle.
- Side effects: When taken orally—and depending on the dosage—unpleasant side effects such as reduced libido and decreased potency may occur. Therefore, medical supervision is necessary, and oral use should be approached with caution or avoided. These side effects are much less common or entirely absent when the medication is administered through scalp injections.
Dutasteride
- Mechanism of action: Dutasteride works similarly to Finasteride but inhibits both isoforms of the 5-alpha-reductase enzyme (Type I and Type II) and has a much longer half-life, resulting in prolonged effectiveness. This makes it more effective at blocking the action of dihydrotestosterone (DHT).
- Application: Administered orally or via injection into the scalp using a very fine needle.
- Side effects: Similar to Finasteride — when taken orally and depending on the dosage, unpleasant side effects such as decreased libido and reduced potency may occur. Therefore, medical supervision is necessary, and oral use should be approached with caution or avoided. These side effects are much less common or completely absent when administered through scalp injections.
Synergy of Medications
The combined use of Minoxidil, Finasteride/Dutasteride, and Botox offers the following advantages:
- Multifactorial effect: The combination targets multiple mechanisms — improving blood circulation (Minoxidil), reducing dihydrotestosterone (DHT) levels (Finasteride/Dutasteride), and relaxing the scalp muscles (Botox).
- Synergistic effects: By simultaneously addressing both hormonal and physical factors, better results can be achieved than with monotherapy alone.
- Individual adaptability: The treatment can be customized to each patient’s specific needs to minimize side effects and maximize effectiveness.
Prevention and Treatment of Hair Loss Using the Body’s Own Substances (Regenerative Medicine)
The treatment methods of regenerative medicine, on the other hand, do not aim to counteract the effects of dihydrotestosterone (DHT) but rather to promote the recovery and regeneration of hair follicles that have become miniaturized and functionally impaired.
Currently, three endogenous (autologous) substances are available for use in regenerative medicine:
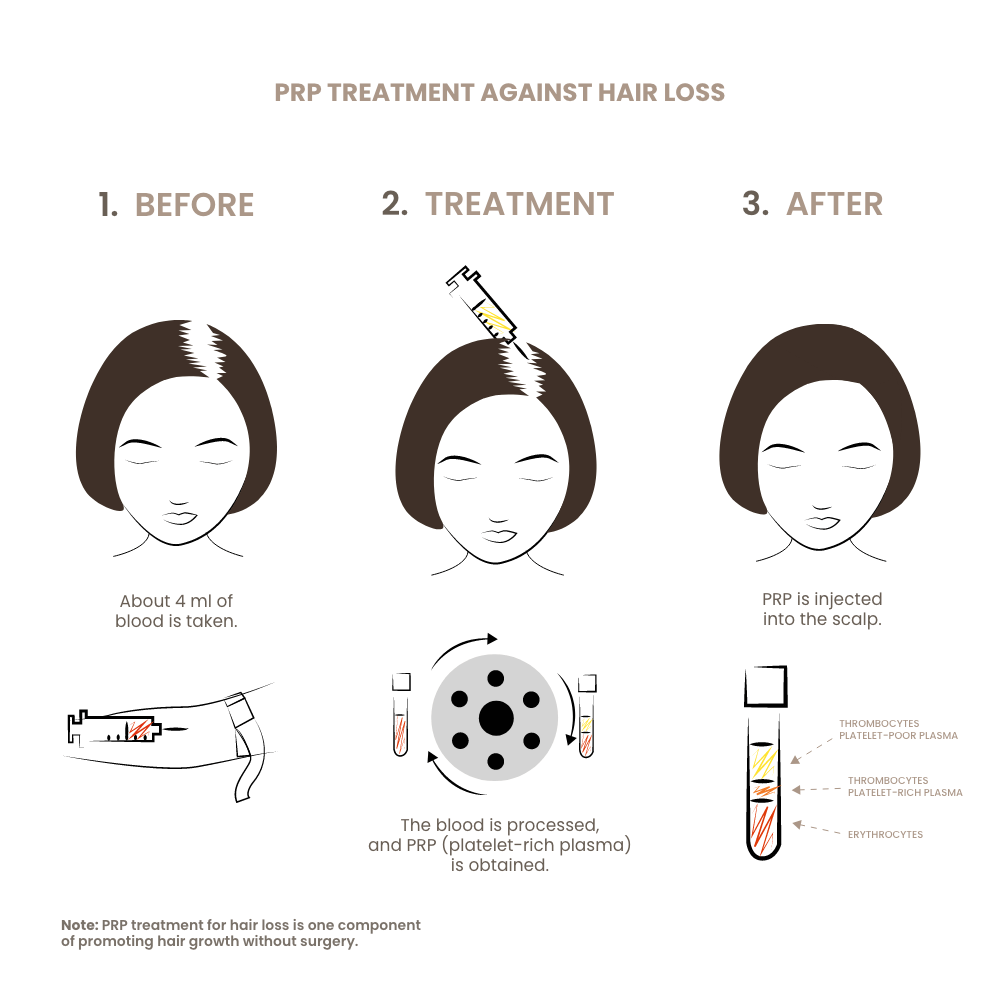
PRP
PRP (plättchenreiches Plasma): Substanz ist schon seit über 30 Jahren in der Medizin bekannt. Man gewinnt sie aus dem Blut, durch Zentrifugation werden die zellulären Bestandteile von der flüssigen Phase getrennt und im Plasma sind dann die Blutplättchen (Thrombozyten) konzentriert. In den Thrombozyten (Blutplättchen) befinden sich Wachstumsfaktoren, wenn man die Blutplättchen in das Gewebe einbringt, dann werden Sie Blutplättchen aktiviert und die Wachstumsfaktoren werden freigesetzt in dem die Zellmembranen undicht werden bzw. platzen. Die Wachstumsfaktoren haben eine sehr starke regenerative Potenz, man kann damit Geschwüre in der Hornhaut zum Appellen bringen, Geschwüre bei offenen Wunden bei Diabetikern, Parodontose zum Appellen bringen, in der Gynäkologie postmenopausale Beschwerden lindern, das Hautbild verbessern, Narben weicher machen, Pigmentflecke reduzieren und vieles mehr. Wenn man PRP in die Kopfhaut spritzt, kann der Haarausfall verlangsamt und auch gestoppt werden, das Haarwachstum wird gefördert werden und es wachsen Haare auch anstellen wieder nach, wo sie bereits ausgefallen waren. In der androgenen Alopezie ist die Erfolgsrate leider nicht sehr hoch, sie liegt bei 10-30 %. Bei der postmenopausalen Alopezie ist Erfolgsrate höher und liegt bei 20-50 %. Beim PCOS-Syndrom ist die Wirksamkeit sogar noch etwas höher, weil die Betroffenen jünger sind.
Zuletzt sei noch erwähnt, dass PRP die Wirkung der Stammzellen des Eigenfett (Nanofett – siehe später) verstärkt.
PRP ist daher ein gewichtiger Bestandteil unseres Therapieansatzes
Nanofat
The somewhat misleading term Nanofat refers to stem cells derived from the body’s own fat tissue. The term is confusing because Nanofat technically does not contain intact (living) fat cells. It entered medical terminology because two Belgian physicians, Tonnard and Verpaele, described in their first publication a substance obtained by intense mechanical fragmentation of autologous fat and simply called it “Nanofat,” referring to a smaller stage in the sequence macro–mini–milli–nano.
Since 2001, it has been known that fat tissue contains high concentrations of stem cells. For comparison: blood contains only about 0.5% stem cells, whereas fat tissue contains between 5% and 10%. Until a few years ago, stem cells from fat could only be extracted through a complex enzymatic process in a laboratory. However, for the past few years, simple, inexpensive, and time-efficient mechanical methods have become available, allowing stem cell extraction within 10–15 minutes after aspirating 10–20 ml of autologous fat.
The aspirated fat is deliberately pressed through a sharp filtration system to destroy the fat cells and release the stem cells from the connective tissue framework of the fat. The resulting product therefore contains destroyed fat cells and stem cells suspended in an emulsion derived from the patient’s own fat. When Nanofat is introduced into the body, it triggers a regenerative process — depending on the surrounding tissue, various types of body cells can develop. Nanofat has a particularly strong regenerative effect on miniaturized hair follicles. However, it is not volumizing and thus not a filler, unlike microfat, which is primarily used for volume restoration.
The mechanism and range of effects of autologous stem cells are almost identical to those of PRP but are significantly superior in their regenerative potential.
Nanofat is therefore an essential component of our therapeutic approach.
Exosomes
Exosomes are tiny vesicles that contain signaling molecules and serve as carriers for the transmission of biochemical messages between cells.
They represent the newest tool in the arsenal of regenerative medicine. Currently, health authorities in Asia, the United States, and Europe are debating which types of exosome-based substances may or may not be approved for medical use. For this reason, it would not be scientifically sound to make definitive statements yet about the effectiveness of exosomes in promoting hair regeneration and growth.
What is certain, however, is that at present only autologous (body-derived) or plant-based exosomes are permitted for use in Europe. Nonetheless, there is already strong evidence suggesting that exosomes will play a significant role in non-surgical hair growth stimulation in the near future.
Basic Principles of Non-Surgical Hair Growth Stimulation
Note: All currently known treatment methods for genetically determined hair loss still cannot eliminate the root cause — the hypersensitivity of hair follicles to dihydrotestosterone (DHT).
All medical treatments address the effects of DHT on the hair follicles: either by increasing blood circulation — thereby reducing the duration and intensity of follicular exposure to DHT — or by inhibiting the enzyme 5-alpha-reductase, which converts testosterone into DHT.
The same applies to the use of autologous substances in regenerative medicine: PRP and nanofat are very effective in promoting hair growth, but they cannot influence the individual sensitivity of hair follicles to DHT.
It therefore follows logically that the treatment of androgenetic alopecia — in both men and women — cannot be a one-time intervention. Once initiated, it must be regarded as a long-term therapy, to be continued as long as the goal is to control hair loss. Depending on the degree of follicular sensitivity and the severity of hair loss, both the dosage and frequency of treatments need to be adjusted.
However, the full range of treatments is not always necessary: if the initial therapy yields a good response, a less intensive and more affordable maintenance therapy may often be sufficient — depending, of course, on the initial condition and the individual’s response to treatment.
Our Therapeutic Approach
The most important foundations of non-surgical hair growth stimulation:
- The earlier the treatment begins, the better the chances of success.
- When deciding to undergo treatment, it is important to understand that this is a long-term commitment: as mentioned several times, the treatment does not correct the genetic hypersensitivity of the hair follicles to dihydrotestosterone (DHT).
Diagnostics
Since there are several other possible causes of hair loss besides genetic factors, these must naturally be ruled out before starting any treatment. This includes a blood test and a medical history assessment (patient consultation).
Analysis and Treatment Planning
During the initial consultation, the scalp is examined under a microscope at various points, and the condition of the hair is documented. This allows us to determine whether hairs in the anagen (growth) phase are still present within the thinning or bald areas, providing insight into the potential success of the therapy.
After analyzing the images, an individualized treatment plan is created.
Therapy – Treatment
Our therapeutic concept for conservative, non-surgical hair loss treatment is based on two approaches:
- Exclusive regenerative therapy with PRP and/or nanofat
- Combined therapy using regenerative medicine, antiandrogenic agents, and circulation-enhancing medications
Explanation:
While treatment with regenerative medicine alone (PRP and/or nanofat) is generally less effective than the combined approach, it is simpler, more affordable, and often sufficient.
As is often the case in medicine, practice is the best proof.
We recommend the combined therapy — integrating regenerative medicine, antiandrogenic medication, and circulation-enhancing agents — when the diagnostic analysis indicates that a more comprehensive approach is necessary.
Procedure
Before starting the treatment, photographs are taken — and again at the end of the treatment.
The regenerative therapy alone is available in two variations:
- PRP only – the “starter package”: Using an injection device, approximately 10 ml of PRP is injected into the scalp at least three times at four-week intervals (unlike most clinics, we always count the number of platelets before injection to ensure that the PRP is truly concentrated), ideally five times every four weeks. If this treatment already produces visible or satisfactory results, a maintenance therapy of one injection every four months is usually sufficient.
- Nanofat and PRP – the body’s own “power version”: First, nanofat is injected into the scalp, mixed with 20% PRP, as the presence of PRP enhances the regenerative potential of the stem cells. About 20 ml of autologous fat is harvested from a donor site under local anesthesia, mechanically processed to destroy the fat cells, and the stem cells are isolated and injected into the scalp. This is followed by four additional monthly PRP sessions. If visible improvement occurs, PRP injections are repeated every four months, and the nanofat injection annually. After the first treatment cycle, the success of the therapy becomes evident. If results are positive, treatment can be continued — sometimes at a reduced intensity — or maintained as is. If the regenerative approach alone is insufficient, combined therapy can be introduced.
The combined therapy of regenerative medicine, antiandrogenic medication, and circulation-enhancing medication is also available in two variations, both lasting 4–5 months per treatment cycle.
- Combination Treatment 1: At defined intervals (weekly or biweekly), antiandrogenic agents (Finasteride/Dutasteride), vasodilators (Minoxidil, Botox), and PRP are injected into the scalp using fine needles. The procedure requires no anesthesia and takes about 10–15 minutes. Between sessions, the scalp is treated with special lotions.
- Combination Treatment 2: At defined intervals (weekly or biweekly), antiandrogenic agents (Finasteride/Dutasteride), vasodilators (Minoxidil, Botox), nanofat, and PRP are injected into the scalp using fine needles. The procedure also requires no anesthesia and takes about 10–15 minutes (nanofat application takes 30–45 minutes). Between sessions, the scalp is treated with special lotions.
After the first treatment cycle, it becomes clear whether the therapy is successful. If results are positive, the treatment may be continued, reduced in intensity, or transitioned to topical maintenance therapy.
Note: The precise sequence of injections, timing, concentration, dosage, and coordination of the administered substances are the result of 15 years of experience in this field.
We therefore kindly ask for your understanding that the exact details of the combination treatment cannot be disclosed.
Costs
- Course with concentrated platelets: The cost of this treatment ranges from €2,100 (3 sessions) to €3,500 (5 sessions).
- Course with nanofat (stem cells from the patient’s own fat) + 3× (5×) concentrated platelets: The cost of a combined nanofat and concentrated platelet treatment is €5,000 (nanofat + 3× concentrated platelets) or €6,000 (nanofat + 5× concentrated platelets).
- Combination treatment 1: 9 sessions involving injections of antiandrogenic, vasodilating, and regenerative agents (3× concentrated platelets, 6× antiandrogens + Minoxidil), plus a topical Finasteride + Minoxidil solution: €6,000; with Botox: €6,500.
- Combination treatment 2: 10 sessions with injections of antiandrogenic, vasodilating, and regenerative agents (1× stem cells + concentrated platelets, 3× concentrated platelets, 6× antiandrogens + Minoxidil) and topical application: €8,500; with Botox: €9,000.
- Combination treatment 3: 12 sessions with injections of antiandrogenic, vasodilating, and regenerative agents (1× stem cells + concentrated platelets, 3× concentrated platelets, 8× antiandrogens + Minoxidil) and topical application: €9,500; with Botox: €10,000.
Note: The success rate of our treatments is very high. Therefore, we offer all our patients a partial refund in case of no visible improvement — 30% reimbursement for combination treatment 1, and 40% reimbursement for combination treatments 2 or 3.
The evaluation of treatment results is based on before-and-after photographs taken no later than one month after the final session. A treatment is considered successful if an increase in hair density is visibly noticeable. The extent of improvement (slight, moderate, or significant) does not matter, as even a minor visible enhancement in density indicates that hair loss has been reduced and the injection therapy has been effective.